Electrophysiological Study of Heart Disorders: What You Need to Know
The human heart is an engineering miracle that works nonstop to pump blood, providing our bodies with oxygen and nutrition.
This important organ is not impervious to faults, though. Heart conditions, commonly referred to as arrhythmias, can obstruct the heart’s rhythmic contractions, with potentially fatal results.
Medical experts use the field of Electrophysiological study of heart disorders, a subfield of cardiology, to comprehend and manage these problems.
The Heart’s Electrical System
It’s crucial to understand the fundamentals of the heart’s electrical system before diving into electrophysiological research.
The electrical impulses that cause the heart to contract are produced internally; it does not rely on outside factors like nerves to do so.
These specialized cells act as the body’s internal “pacemaker” system, initiating and transmitting electrical impulses to keep the heart beating in time and rhythm.
The sinoatrial (SA) node, the atrioventricular (AV) node, the bundle of His, and the Purkinje fibers are the main elements of the heart’s electrical system.
Each pulse is started by the SA node, also referred to as the natural pacemaker. The atria contract as a result of the electrical impulses it delivers, pumping blood into the ventricles.
As a gateway, the AV node temporarily reduces the electrical impulses to give the ventricles time to fill with blood.
The quick transmission of the impulses to the ventricles through the bundle of His and Purkinje fibers causes them to vigorously contract, pumping blood to the lungs and the rest of the body.
What Are Heart Disorders?
When the heart’s electrical circuitry is disrupted, cardiac conditions known as arrhythmias result. Heart rhythm irregularities can result from this disturbance, which can take many different forms. Common arrhythmias include the following:
1. Atrial Fibrillation (AFib)
One of the most common arrhythmias, AFib is characterized by erratic and fast atrioventricular contractions.
Blood can accumulate in the atria as a result of this uneven pulse, raising the risk of blood clots and stroke.
AFib is frequently linked to diseases including hypertension, diabetes, and heart disease and can be episodic or permanent.
2. Ventricular Tachycardia (VT)
The ventricles, the heart’s bottom chambers, are the source of the dangerous arrhythmia known as VT (Ventricular Tachycardia).
It is characterized by frequent, fast contractions of the ventricles that, if left untreated, can be fatal. People with a history of heart disease or a heart attack frequently get VT.
3. Bradycardia
The opposite of tachycardia, bradycardia, is characterized by an unusually slow heart rate, usually less than 60 beats per minute.
Conduction system anomalies or SA node dysfunction might also contribute to this disease. Bradycardia can, in extreme circumstances, result in cardiac arrest or fainting.
4. Supraventricular Tachycardia (SVT)
SVT (Supraventricular Tachycardia) refers to a collection of arrhythmias that start above the ventricles. It results in an accelerated and steady heart rate and can bring on palpitations, lightheadedness, and chest discomfort.
SVT episodes can be short or protracted in duration.
5. LQTS (Long QT Syndrome)
LQTS is a hereditary condition that interferes with the electrical function of the heart. It increases the risk of abrupt cardiac arrest and can cause irregular heartbeats.
Electrocardiogram (ECG) results frequently show a longer QT interval in people with LQTS.
The Role of Electrophysiological Study of Heart Disorder Diagnosis
An extensive analysis of the heart’s electrical activity is necessary for the diagnosis of cardiac conditions. Electrophysiology (EP) plays a role in this.
Cardiology’s subspecialty of electrophysiology focuses on understanding the electrical characteristics of the heart as well as identifying and treating arrhythmias.
1. Electrocardiogram (ECG)
The electrocardiogram, sometimes known as the ECG, is the basis of electrophysiological study of heart research.
This non-invasive examination captures the electrical activity of the heart across a short- to medium-term time span.
It offers important knowledge regarding the conduction system, rhythm, and pace of the heart.
Electrodes are affixed to the skin’s surface at specified points on the body during an ECG. These electrodes identify electrical cardiac impulses and plot them as waveforms on a graph.
Doctors can diagnose a variety of arrhythmias by examining the ECG for irregularities in the heart’s electrical pattern.
2. Holter Monitoring
The electrical activity of the heart is captured in a conventional ECG, however certain arrhythmias are erratic and may not be detected in a quick recording. In these circumstances, Holter monitoring is used.
In order to record intermittent arrhythmias, this entails carrying a portable ECG instrument for a prolonged length of time, often 24 to 48 hours.
Holter monitoring gives doctors the option to watch the heart’s electrical activity over a longer period of time, increasing the likelihood that anomalies won’t go unnoticed.
3. Event Monitoring
Even less common arrhythmias are treated with event monitoring. Similar to a Holter monitor, this device is worn for a longer period of time—typically weeks to months.
When they encounter symptoms, patients can activate the device to record their heart’s electrical activity, enabling a focused evaluation of arrhythmias.
4. Electrophysiological Studies (EPS)
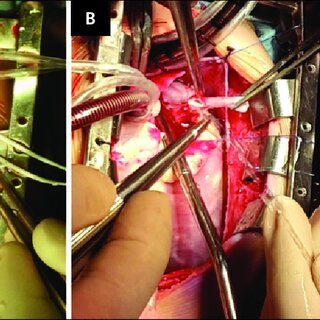
Electrophysiological investigations (EPS) may be carried out when the aforementioned non-invasive procedures are insufficient to provide a conclusive diagnosis or when more precise information is required.
In order to access the heart’s chambers during EPS, electrode-equipped catheters are inserted into blood arteries.
As soon as the catheters are inserted, they may capture electrical impulses coming directly from the heart, giving precise information on the electrical activity of the organ.
EPS can also help identify the precise location of abnormal electrical pathways responsible for certain arrhythmias, which is crucial for planning treatment strategies.
Related Article: Advancements in Targeted Therapies for Hematological Malignancies
Treatment Approaches Based on Electrophysiological Study of Heart Findings
In addition to helping with diagnosis of cardiac conditions, electrophysiological investigations are essential in choosing the best possible course of therapy.
The following treatments are possible for arrhythmias, depending on their nature and severity:
1. Medications
Medication that helps control the electrical activity of the heart can be used to treat several arrhythmias.
Beta-blockers and calcium channel blockers, for instance, can lower heart rate while antiarrhythmic medications can assist keep rhythm regular.
The precise arrhythmia and the patient’s general health will determine the drug to be used. Which drug is most likely to be successful can be determined with the use of electrophysiological investigations.
2. Catheter Ablation
A common minimally invasive technique used in electrophysiological studies is catheter ablation. Catheters are used to administer radiofrequency radiation or freezing (cryoablation) to the specific area of the heart where the arrhythmia is occurring.
Catheter ablation can successfully stop the arrhythmia by ablating or obliterating the aberrant electrical pathways, offering many patients a long-term remedy.
During this technique, electrophysiological investigations are crucial because they enable the electrophysiologist to precisely map the heart’s electrical circuits and identify any troublesome regions.
3. Implantable Devices
Implantable devices may be advised in situations of severe or life-threatening arrhythmias. These gadgets can assist in controlling the heart’s rhythm and avoiding unexpected cardiac arrest.
There are two main categories of implanted devices:
– Pacemakers: Pacemakers are inserted beneath the skin and wired to the heart using leads. They continually track the electrical activity of the heart and send electrical impulses when the heart rate slows down too much.
The placement of pacemaker leads is frequently guided by electrophysiological investigations in order to maximize their efficiency.
– Implantable Cardioverter-Defibrillators (ICDs): Similar to pacemakers, ICDs also have the capacity to shock the heart violently in order to stop life-threatening arrhythmias like ventricular tachycardia or ventricular fibrillation.
Studies on electrophysiology aid in choosing the best times and ways to tune these devices for optimum operation.
4. Surgery
Surgical procedures may be required in some difficult situations, particularly when arrhythmias are linked to structural cardiac issues.
To stop arrhythmias, surgical techniques may entail changing the electrical or structural components of the heart.
By giving exact details regarding the location and kind of the arrhythmia, electrophysiological investigations are frequently used to assist surgical planning.
When all other therapeutic alternatives have been tried or are ineffective, surgical techniques are frequently taken into account.

The Advantages of Electrophysiological Studies of Heart Disorders
By providing numerous important benefits in the detection and treatment of cardiac diseases, electrophysiological investigations have changed the area of cardiology:
1. Precision Diagnosis
The electrical activity of the heart is precisely and thoroughly described by electrophysiological research.
Accurate diagnosis of arrhythmias and knowledge of their underlying causes are essential for enabling healthcare professionals to customize treatment regimens for specific patients.
2. Treatment guidance
Arrhythmias are diagnosed via electrophysiological investigations, which are also used to provide therapy recommendations.
They aid electrophysiologists in selecting the best course of treatment, be it medicine, catheter ablation, implanted technology, or surgery.
The likelihood that a patient will benefit from treatment is increased by this tailored approach.
3. Mapping Complex Arrhythmias
Due to their intricacy, certain arrhythmias can be difficult to identify and treat.
Doctors can pinpoint the precise location of faulty electrical pathways by using electrophysiological investigations to create accurate electrical maps of the heart.
This is especially helpful for situations like ventricular tachycardia and atrial fibrillation.
4. Minimally Invasive Procedures
Numerous therapies may now be carried out with a minimum of invasiveness because to electrophysiological research.
Open-heart surgery is not always necessary for procedures like catheter ablation, which lowers the risks, complications, and recovery time involved with conventional surgical techniques.
5. Research and Advancements
Our knowledge of the heart’s electrical mechanism has advanced significantly thanks to electrophysiological investigations.
They have contributed to the development of new treatment strategies, medications, and devices for managing arrhythmias.
Ongoing research in electrophysiology continues to drive innovation in cardiology.
Risks and Considerations
While electrophysiological studies are highly valuable in diagnosing and treating heart disorders, they are not without risks and considerations:
1. Invasive Nature
Invasive electrophysiological tests necessitate the insertion of catheters into the body. There are hazards associated with this, such as infection, bleeding, and harm to blood vessels or the heart.
Although often small, these risks are exceeded by the potential advantages of proper diagnosis and therapy.
2. Radiation Exposure
Fluoroscopy, a form of X-ray, is frequently utilized during electrophysiological tests to view the catheters within the body.
Long-term radiation exposure has its own hazards, especially for medical professionals who conduct these operations often. Radiation exposure is attempted to be as low as feasible.
3. Complications
Complications are possible with any medical operation, as well. These could include infections, blood vessel damage, or arrhythmias brought on by the operation.
Before participating in an electrophysiological research, patients should talk with their healthcare practitioners about the advantages and disadvantages.
4. Patient Cooperation
When employing conscious sedation or local anesthetic for electrophysiological tests, patient participation is crucial.
To guarantee the procedure’s effectiveness and safety, patients must maintain their stillness and adhere to instructions.
Conclusion
The understanding of the electrical system of the heart gained through electrophysiological investigations has revolutionized the diagnosis and treatment of cardiac diseases.
These investigations allow for accurate diagnosis, direct treatment choices, and have sparked the creation of ground-breaking treatments that enhance the quality of life for millions of people who suffer from arrhythmias.
While electrophysiological testing does have certain hazards, the precision and individualized treatment they may provide far exceed these concerns.
The discipline of electrophysiology is anticipated to witness additional improvements in diagnostic and therapeutic approaches as technology develops, providing even more hope for those with heart diseases.
If you or a loved one are experiencing symptoms of an arrhythmia, consult with a cardiologist to explore whether an electrophysiological study may be the next step in your journey towards a healthier heart.




